Revolutionizing the pharmacy benefit experience
At Optum Rx, we’re harnessing cutting-edge AI and advanced technology to transform the pharmacy benefit experience. Through Optum AI assistants, we are making pharmacy benefits as easy as a conversation. And we’re not just meeting expectations — we’re anticipating needs, reducing effort, and empowering members, providers and clients to achieve better outcomes.
Our AI and advanced technology initiatives are built around preventive, predictive and ease-of-use capabilities that ensure seamless, personalized interactions across every touchpoint. From proactive models that resolve member issues before they’re even noticed to systems that fast-track prior authorizations and claims processing, we’re delivering smarter, faster, and more personalized pharmacy support.
Using advanced technology to enhance pharmacy experiences
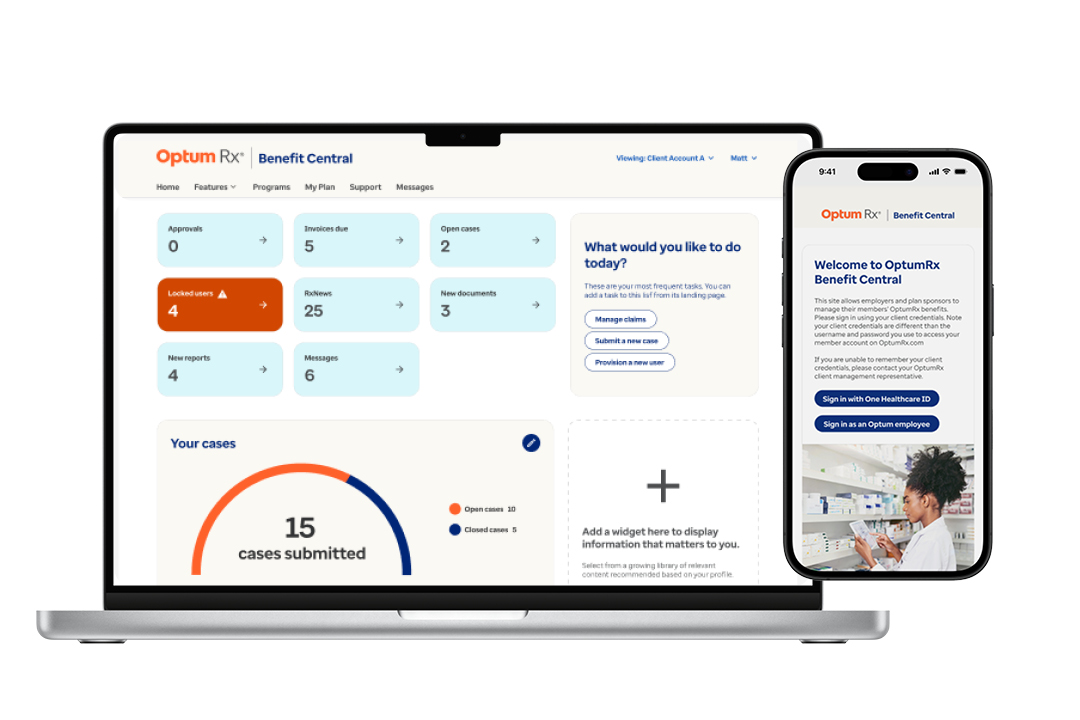
Benefit Central – Plan management made easy
With Optum Rx Benefit Central™, clients can experience 3x faster claims processing than competitors, flexible plan builds in under 10 minutes, and powerful trend management with AI plan diagnostics.

Automated support removes the need to call
2.4 million member calls were successfully resolved in 2024 using AI-powered natural language voicebots, with plans to eliminate an incremental 1 million calls in 2025.2

Focused and direct support for complex issues
AI that predicts and resolves possible member issues, eliminating 80% of potential call escalations. Expecting 56,000 fewer complex member calls, with 21,000 member escalations proactively avoided in 2025.3

AI-powered fraud detection returns dollars to clients
As fraud schemes evolve, we’re continuously enhancing our pharmacy claims detection model. Our AI-enhanced fraud, waste and abuse audits have resulted in $2M in financial recoveries per client.4
Integrated AI-powered prior authorization
We are the only pharmacy benefit manager integrated with Surescripts® Electronic Health Records system, enabling over 65% of electronic prior authorizations to be auto-decisioned in real time with 100% accuracy and approvals in less than 30 seconds.5
On-demand webinars
Advanced Tech in Pharmacy
See how we're harnessing AI and advanced digital solutions to make care more transparent, simple, and affordable at scale.
Innovating Responsibly with AI
Discover how we’re using predictive, generative, and agentic AI to create smarter, more personalized experiences for members and clients.
Industry insights

Article
From predicting drug trend to earlier fraud protection, see how we’re leveraging AI to improve operations for clients and members.
Article
In our latest podcast, two AI experts discuss how Optum Rx is leveraging artificial intelligence while prioritizing privacy and security.

We offer insights into the ways Optum helps health plans solve cost, quality, member experience and compliance challenges.
Complementary solutions
Optum Rx Benefit Central™
Benefit Central is your cloud-based, self-service platform designed to streamline plan management — because your time is important.
Simplifying the pharmacy benefit experience
We are creating a simplified, more connected health care experience for you, your members, and the providers who care for them.
Driving appropriate utilization of medications
We are committed to helping members stay adherent to medications while addressing the industry challenges that prevent them from doing so.
- Enterprise ranking in Fortune AIQ 50 ranking
- 2024 Optum Rx internal analysis.
- Ibid
- Ibid
- Optum Rx and Surescripts data. April - June 2024.


