
Coordinate member care and treatment in non-hospital settings
The Optum Home & Community Full Population Management solution is a full-risk arrangement designed to provide in-home health assessments and care for Dual Special Needs Plan (D-SNP) members. Highly credentialed community-based providers such as nurse practitioners coordinate member care and treat members in non-hospital settings.
This results in industry-leading engagement, impressive health and quality outcomes and stronger financial results for payers.
Deliver expert care to D-SNP members in their homes and communities
A better way to reach your D-SNP members
Our population health management platform deploys highly credentialed, interdisciplinary care teams who treat members in their homes and communities, working together with their existing PCPs and specialists.

Setting a new standard in care delivery
With risk-stratified care planning, members are identified in one of three risk categories, based on 950 input factors. Each category guides clinical actions to meet the member where they are and manage their changing health needs.

Comprehensive in-home health assessments
We provide in-home health assessments to capture, diagnose and drive medical management, including full physical exams, environmental and behavioral screening, prescription medication review and more.

We’ve spent 10 years improving and scaling our fully NCQA-compliant care model. Today we serve 1.4 million D-SNP members.
Key benefits
Eligible members receive a full range of benefits to give them the targeted, community-based care they need.
Annual in-home health assessments
Provide comprehensive annual assessments for members in the comfort of their home.
Home-based medical care
Enhance clinical management and longitudinal care for the highest-risk members.
Care management
Delegate care management for the entire health plan, including contractual and regulatory compliance.
Star ratings and care gap closure
Improve quality measures and reduce costs.
Our next-level care teams
- Chronic disease management
- Advanced care planning
- Gaps in care closure and accurate documentation
- Geriatric care
- Change in condition management
- Member and facility support after hours
- Direct admission to skilled nursing facility (SNF)
- Urgent episodes
- Care plan development
- Post discharge follow-ups
- Functional assessments
- Medication reconciliation
- Central point of contact for member, PCP and care team
- Benefit access resource
- Community health
- Care coordination
- SDOH needs
- Social work
- Gaps in care closure and ongoing medical management
- Pharmacist; outreach and ongoing Rx management
- Transition of care team; post-acute follow-up and MOC
- Palliative end-of-life advanced planning and hospice
- Behavioral health
- Virtual care
- Tech-enabled workflows
- Predictive analytics
- 24/7 provider call center
- New market implementation
- Scheduling optimization
- Clinical education
Industry insights
White paper
A Yale Medicine study shows how in-home health assessments can help Medicare Advantage members get the care they need.
![How an Optum Care Coordinator Works [Video]](/content/dam/o4-dam/resources/videos/ditl-lutheran-home-testimonial-video/ditl-lutheran-home-testimonial-thumbnail-1080x720.jpg)
Video
Supporting care, reducing stress, and serving as a point-of-contact are just a few of the benefits care coordinators offer.
![The Impact of In-Home Health Assessments [Guide]](/content/dam/optum-dam/images/business/insights/senior-woman-in-home-nurse-visit-1080x720.jpg)
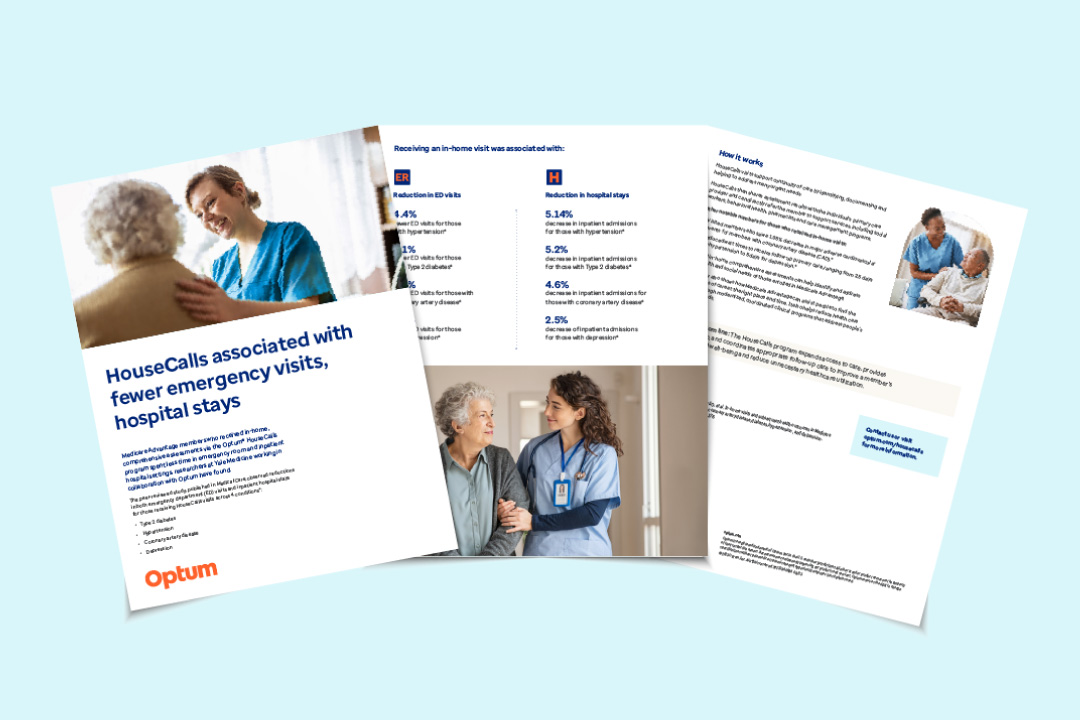
Guide
Learn about the benefits of HouseCalls assessments with these 5 fast facts.
Product information and resources
-
Download fact sheet
PDF
Fact sheet
Full population management solution overview
Read our comprehensive fact sheet to see how our full population health management solution can result in better care and better results for your D-SNP members.
Complementary solutions
HouseCalls
We conduct annual in-home clinical assessments, including health history, medication review, physical exams, and necessary labs and screenings as needed to address health risks.
Post-Acute Care Solutions
We help members transition from acute care to the next appropriate site of care, enhancing clinical outcomes and members’ experience.
Home & Community
We deliver personalized, whole-person care to older adults in the comfort of their home or community, supporting aging in place through various coordinated care options.
