Better plan management
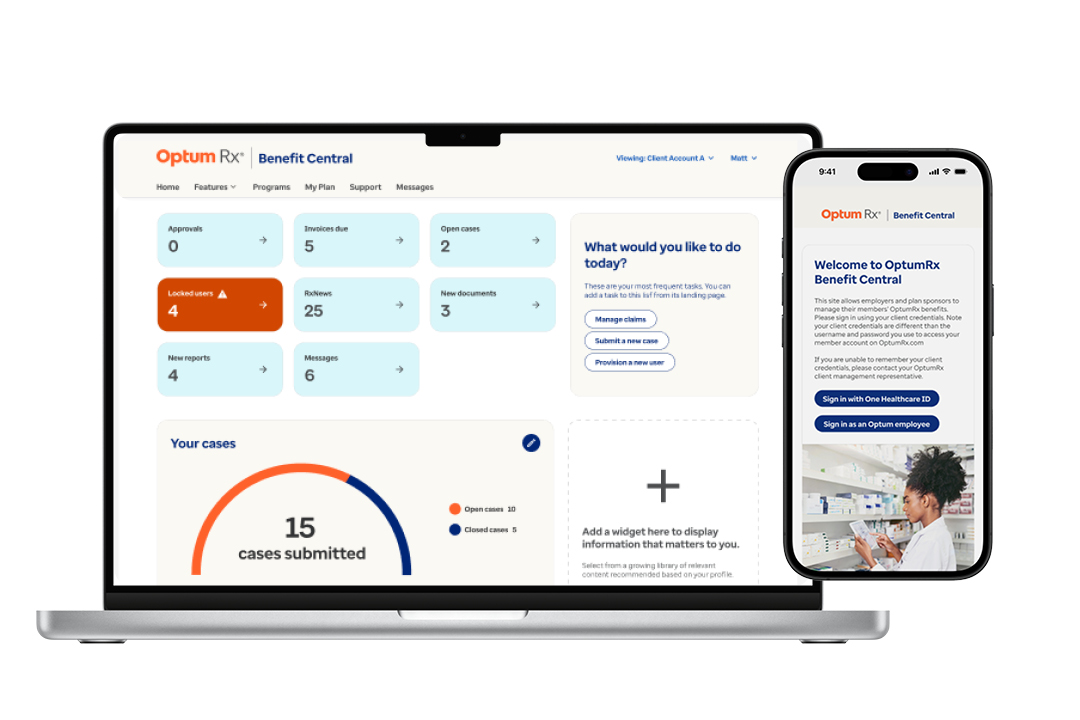
Introducing Benefit Central, a one-stop, self-service client platform for better plan management. This cloud-based ecosystem connects industry-leading benefit capabilities, offering tools for dynamic reporting and streamlined plan management. From member servicing and claims processing to service requests and issue resolution, everything is integrated into one intuitive platform.
Benefit Central's simplified interface design allows quick access to frequently used claim details, leveraging the RxClaim system's size, capabilities, flexibility and adjudication volume. It also includes a proprietary cloud-based onboarding system inspired by leading online experiences, transforming implementation steps into push-button processes completed in minutes with high quality and accuracy.
Automation and technology ensure newly implemented plan designs deliver expected outcomes. Clients can access powerful, on-demand reporting with dynamic, real-time data, providing actionable insights for informed decision-making across drug details, trend drivers and member information.
Streamline pharmacy benefit management for clients

Enhanced transparency
Benefit Central offers detailed insights into pharmacy benefit plans, costs and member health data, empowering clients to make informed decisions and manage plans confidently. Real-time data and actionable insights help clients stay ahead of issues and optimize benefit strategies.

User-friendly design
The platform's intuitive, mobile-first interface simplifies member management tasks, ensuring a seamless client experience. This user-friendly design provides seamless navigation and task performance, reflecting Optum Rx's commitment to expert support and innovative solutions.

Dynamic reporting
Benefit Central provides real-time data via a redesigned portal with interactive dashboards and robust reporting tools. Users gain insights across claims, members, drugs, trend drivers and performance metrics, helping identify opportunities to better manage prescription drug costs and utilization.

Member servicing
Clients can look up member and claim history, update member eligibility and leverage robust reporting, all within Benefit Central. We continually invest in infrastructure updates and new functionality, including Price Edge, which ensures the best medication prices and provides prior authorization status updates.

Self-service capabilities
Benefit Central empowers clients with self-service tools for invoice management, issue resolution, document management, user onboarding and reporting. These capabilities enable clients to manage tasks independently, reducing administrative burdens and enhancing efficiency.
Key benefits
Clients can view personalized dashboards, see transparent pricing and reporting, and more.
Claim and member management
A centralized claims repository offers rapid data extracts and transparent pricing and reporting.
Document management
A single document repository allows for collaboration.
Service request experience
Submissions and tracking are simplified with personalized dashboards.
Clinical publications
Users have access to the latest drug safety communications and clinical publications.
User management
Self-service user setup and management enhance flexibility and autonomy.
PBM software to make decisions all in one place
Optum Rx Benefit Central is designed to provide everything clients need to optimize their plan management — all in one place. Discover how Benefit Central delivers a top-tier self-service client experience by leveraging intelligent technology, advanced analytics and a comprehensive approach to transparency.
Industry insights
![A Seamless Pharmacy Benefit Change? [Case Study]](/content/dam/optum-dam/images/business/pharmacy/team-meeting-at-desks-1080x720.jpg)

Article
Discover how digital communications can increase member engagement and lower the cost of care.

Article
Discover our latest innovation to the PA process — PreCheck Prior Authorization — which reduces approval times, appeals and denials.
Complementary solutions
Simplifying the pharmacy benefit experience
We are creating a simplified, more connected health care experience for you, your members, and the providers who care for them.
Driving appropriate utilization of medications
We are committed to helping members stay adherent to medications while addressing the industry challenges that prevent them from doing so.
Using data to improve health outcomes
Everyone deserves access to affordable healthcare. Learn how we're using data and analytics to identify disparities and improve health outcomes for pharmacy members.

