What makes the Optum Rx PBM experience unique?
We're committed to creating a more connected pharmacy benefit management (PBM) experience through access, affordability and advocacy — for you, your members and the providers who care for them.
Plan sponsors have been switching to Optum Rx pharmacy benefit management for more than 25 years because they get value — well beyond a drug’s price. And we guarantee a smooth transition with 100% of client satisfaction guarantees met for 1/1/24.1
Automating and digitizing the pharmacy benefit journey
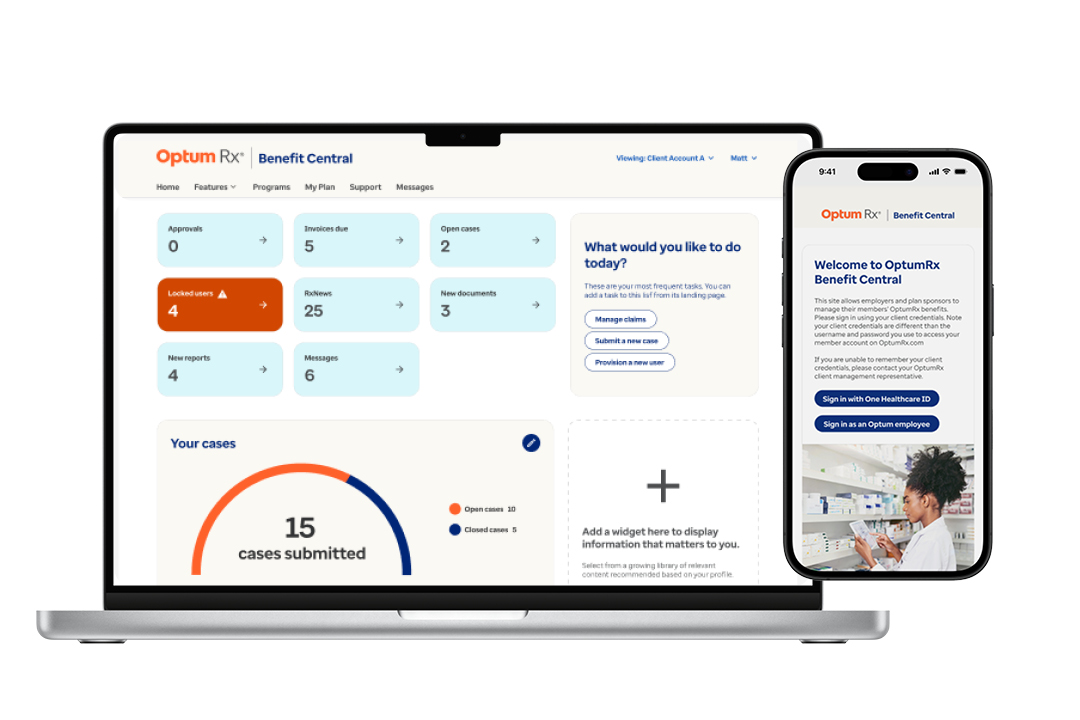
Introducing Optum Rx Benefit Central™
Industry-leading benefit management capabilities
Benefit Central offers enhanced onboarding, plan build automation, seamless adjudication and reporting, automated benefit testing and proactive drug management. These capabilities help you optimize pharmacy benefits across your entire population for a streamlined and efficient experience.
Transforming the experience with PreCheck
Automate the prior authorization process
Our industry-first innovation, PreCheck Prior Authorization expedites prior authorizations, decreasing turnaround times to under 30 seconds.2 With PreCheck MyScript, members can save an average of $214, and clients save $546 per switched medication.3

MyScript Finder shares real-time cost savings
Increasing awareness of medication cost and coverage
Members can access MyScript Finder via the online portal or mobile app and get alternative medication suggestions, the lowest-cost option prior to the prescription being filled, accurate cost by pharmacy and more. Members who switch their medication save an average of $90.4

Taking the paper out of member communications
Fast, frictionless and environmentally-friendly
Consumers expect digital-first experiences for managing their prescriptions. And, while digital promoters have 1.3 more prescriptions per year, they are 1.5 times less likely to cancel a prescription, 8 times less likely to have encountered an issue and have a 3% higher continuity of care.5

Optum Rx’s implementation process was extremely thorough. The team was professional and very good at their job. This was the smoothest transition we have ever gone through.
SVP of Benefits, Large Freight Line Employer Group
How we support the member experience
We guide members every step of the way, making it easy for them to get the medications they need at the prices they can afford.
Eliminating up to 25% reauthorizations
We’re eliminating up to 25% of reauthorizations – more than 10% of overall pharmacy prior authorizations – to simplify access to prescription drugs.
Less than 30 second prior auth approvals
PreCheck Prior Authorization, an industry-first innovation, reduces the turnaround time to under 30 seconds6.
Real-time prescribing details for doctors
PreCheck MyScript gives doctors real-time, plan-specific medication details at the point of prescribing, saving members $214 on average7.
Medication savings alerts for members
Proactive Savings Alerts identify savings opportunities and alert members directly, saving them $42 on average per 30-day script8.
Award-winning communication plan
Empower members to use their pharmacy benefit plan
Our personalized communications start 60 days before go-live and include:
- Welcome materials
- Enrollment support with a pharmacy network directory
- Covered drug list and drug pricing tool
- Transition advocate calls designed to help manage any medication changes

Industry insights

Article
Discover our latest innovation to the PA process — PreCheck Prior Authorization — which reduces approval times, appeals and denials.

Article
Hear from a leader's perspective on how to manage polypharmacy.
![A Seamless Pharmacy Benefit Change? [Case Study]](/content/dam/optum-dam/images/business/pharmacy/team-meeting-at-desks-1080x720.jpg)
Complementary solutions
Driving appropriate utilization of medications
We are committed to helping members stay adherent to medications while addressing the industry challenges that prevent them from doing so.
Optum Rx Benefit Central™
Benefit Central is your cloud-based, self-service platform designed to streamline plan management — because your time is important.
- Optum Rx. 1/1/24 commercial client implementation data.
- Optum Rx. Commercial book of business. January–December 2023.
- Ibid.
- Optum Rx. Internal analysis. January - September 2025.
- Optum Specialty Pharmacy. Internal data. 2023.
- Optum Rx and Surescripts data. April - June 2024.
- 2025 internal analysis (January – June).
- 2024 internal analysis.

