Minimize payer-provider friction
Streamline payment processes and increase transparency
At Optum, we recognize the critical need for timely and accurate provider payments, as well as controlling costs. The complexity of processing Medicaid claims can lead to unnecessary expenses, administrative burdens, and provider dissatisfaction, potentially affecting clinical outcomes. Our collaborative approach with providers, agencies and stakeholders is designed to improve accuracy and transparency.

Featured products

New to Medicaid, familiar to providers
Advanced Communication Engine (ACE)
Already in use in the commercial space across all 50 states via Medicare MACs, this powerful electronic data interchange (EDI) solution addresses claims denials through proactive messaging to providers. It also integrates with your data warehouse or Optum-hosted datamart to offer real-time analytics on claim transactions.

Policy edits may already be embedded
Claims Editing System (CES)
This is a scalable technology that can enhance claims accuracy, increase savings, and improve compliance through comprehensive content integration. The system has a library of 250 million Medicaid code editing combinations, including historical and date sensitive editing and automated clinical coding and billing error checks.

Designed to implement without disruption
Claims Audit Platform (CAP)
This platform offers predictive analytics and a robust case management system to detect and prevent improper Medicaid payments before they occur. It helps with timely and accurate reimbursements while minimizing the risk of fraud, waste and abuse.
Key benefits
We provide states with flexible, customizable options to meet their unique needs. Choose and combine individual solutions within the suite and adapt them.
Reduced administrative expenses
Address improper claim denials, proactively identify potential denials before adjudication and provide guidance to providers.
Managed care transaction visibility
We can provide direct insight into MCO and provider payment performance, including the types and timing of claims being processed, rejected and denied.
Identify and prevent fraud
Post-adjudication review provides capabilities that help states effectively target suspect claims for various billing issues.
Lower administrative costs around adjudication
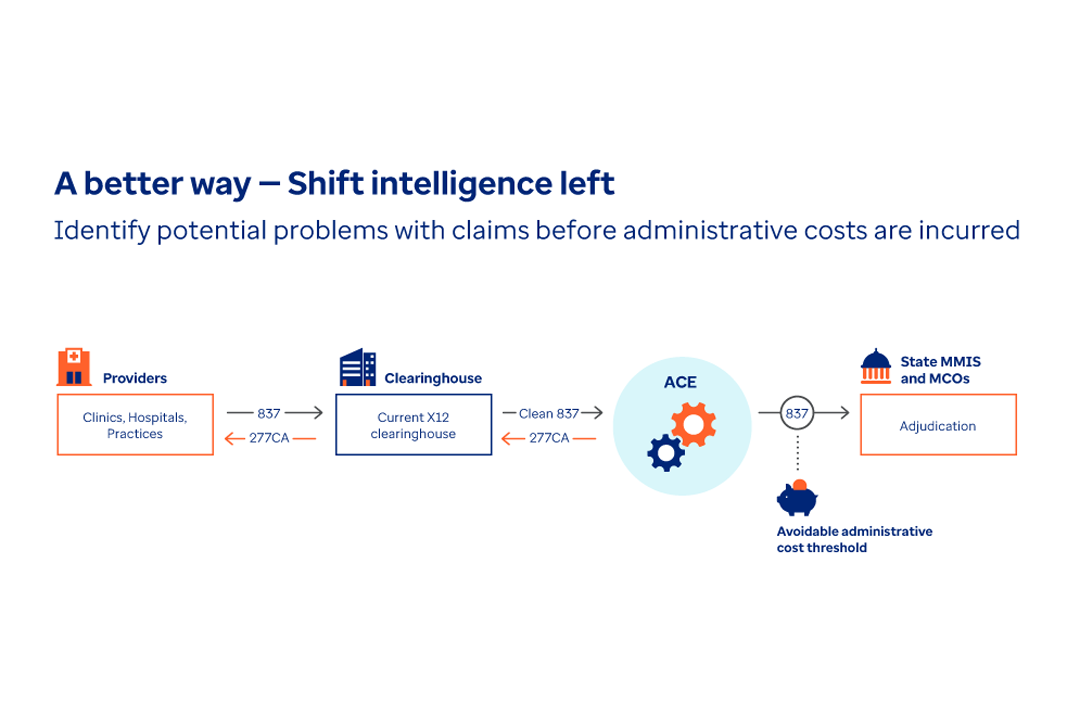
Taking data from providers through the clearinghouse to the ACE dashboard allows states to lower administrative costs around adjudication.
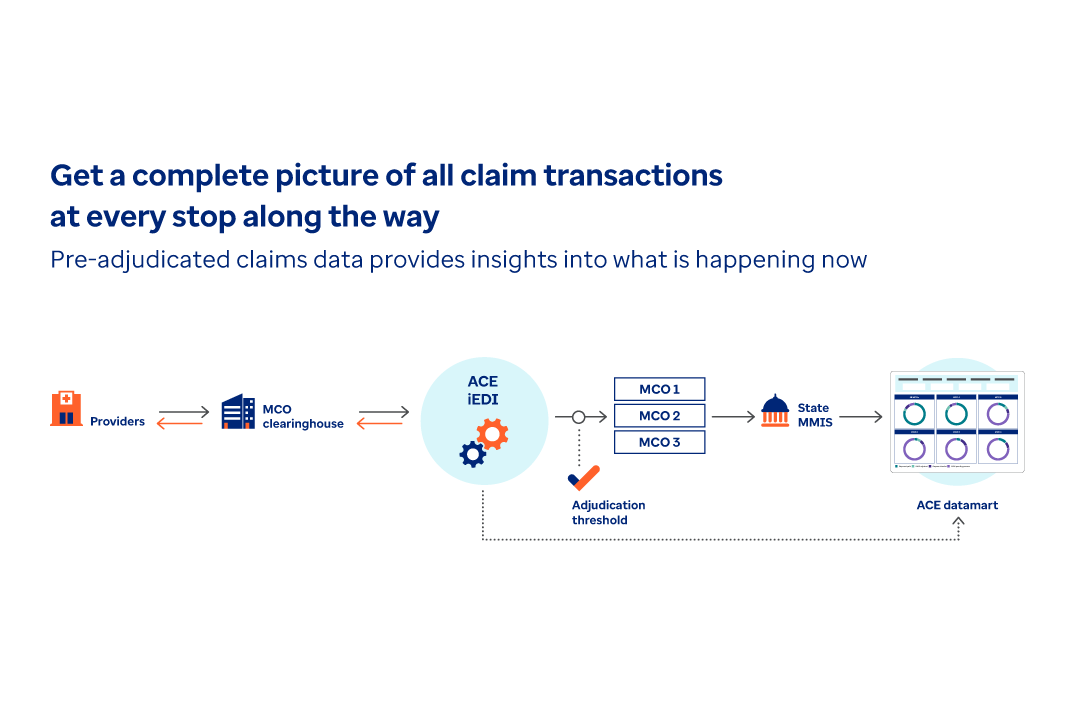
See pre-adjudicated claims data in a dashboard
Provider data flows into the MCO clearinghouse, and the ACE solution allows states to see the pre-adjudicated claims data in an ACE summary dashboard.
Additional product highlights
ACE edits can be tailored to meet the unique needs of each agency. By identifying and rectifying claim issues early in the process, agencies can minimize the need for rework and reduce administrative costs, improving both processing times and provider satisfaction.
- Identify problematic or “certain to deny” claims before costs are incurred.
- Deliver timely notifications with clear instructions on fixing claim errors.
- Influence provider behavior with insights into billing patterns, gaps in care and credentialing status.
By leveraging ACE within their EDI stream and integrating it with an Optum-hosted data warehouse or a stand-alone datamart, states get near real-time insights into current transaction activities. This eliminates the need to wait months for outdated encounter data.
Our time-tested prepay analytics integrate with your adjudication flow to identify potential fraud before payment. Post-pay analytics can be added to enable thorough examination of provider, member and claims data after payment and adjudication for fee-for-service and managed care.
Industry insights

Article
Two AI experts share insights on how we’re using AI and advanced technology to improve everything from trend prediction to member services.

Article
In this conversation, get a peek into upcoming solutions and technologies designed to address high-cost medications.
Article
In our latest podcast, two AI experts discuss how Optum Rx is leveraging artificial intelligence while prioritizing privacy and security.
Complementary solutions
One Assist
Our AI-enabled contact center solution helps states connect providers and members to the answers they need.
Provider Management Services for Medicaid Agencies
Provider Management Services improves the way Medicaid agencies manage provider relationships and administrative tasks.
Program Operations
Transform your state’s operations with modern technology complemented by services.
