How pharmacy benefit managers power medication affordability
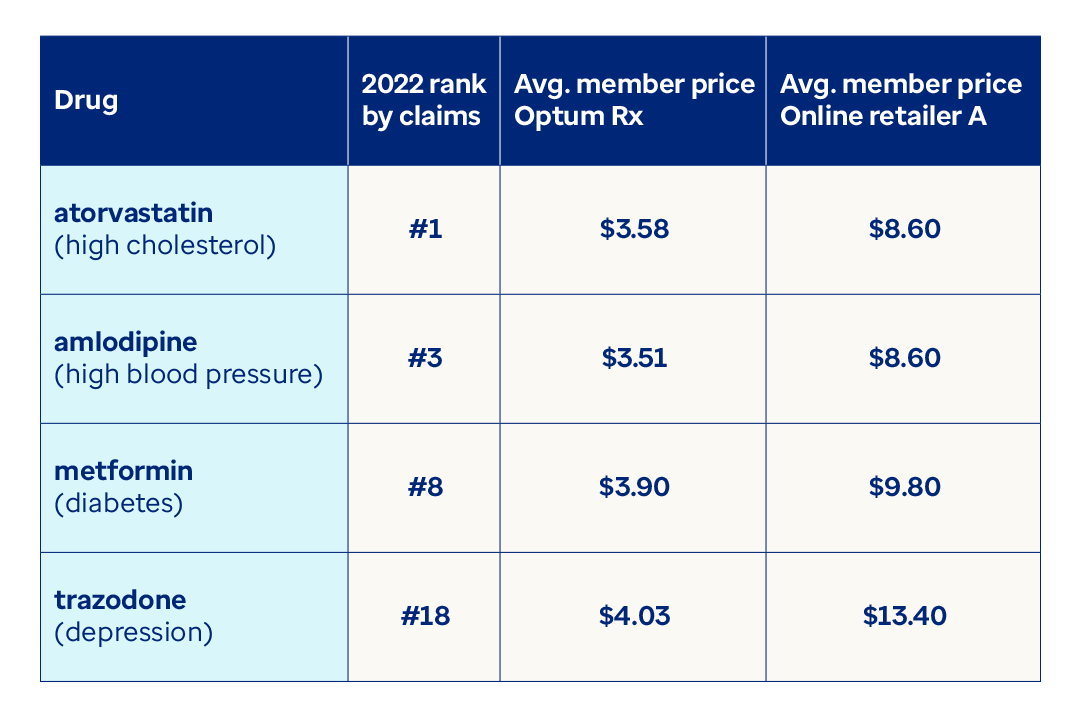
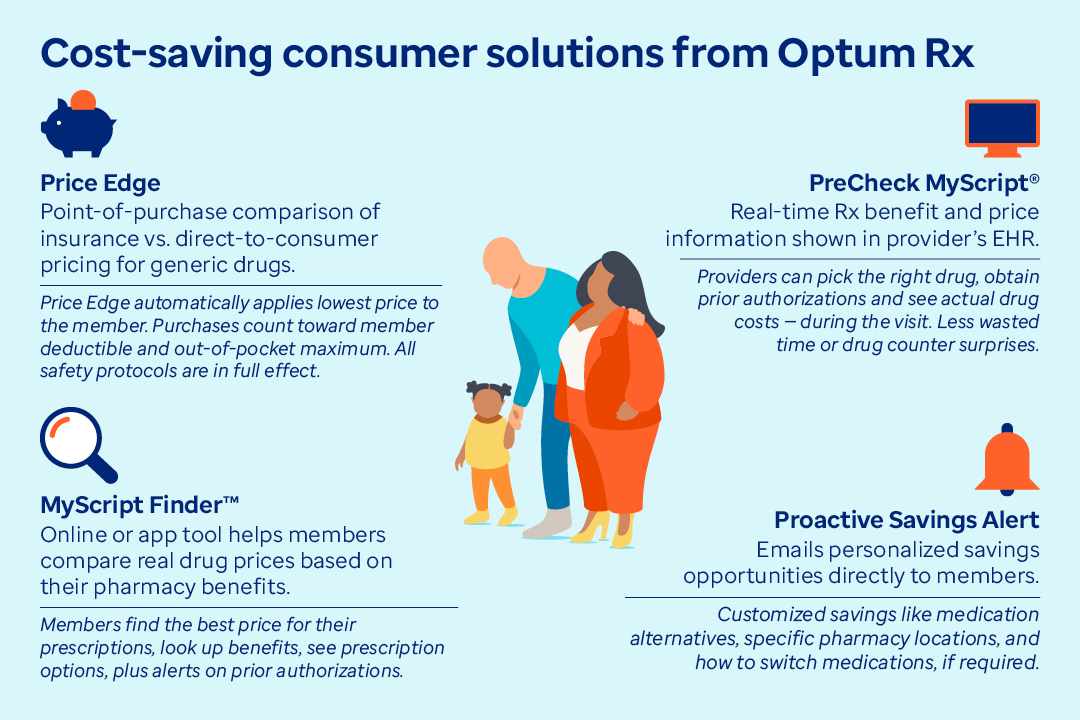
As drug prices continue to rise, Optum Rx is creating innovative solutions that provide affordable access to medications. And yet, there is still a lot of confusion and misinformation around the role of pharmacy benefit managers (PBMs).
Most prominent are the different legislative inquiries investigating PBM activities.1 In addition, the pharmaceutical makers have tried to position PBMs as "middlemen" responsible for driving up the cost of drugs.2
In fact, pharma has by far the biggest lobbying operation in the U.S., spending $374 million in 2022 — nearly 70% more than the next ranked industry.3
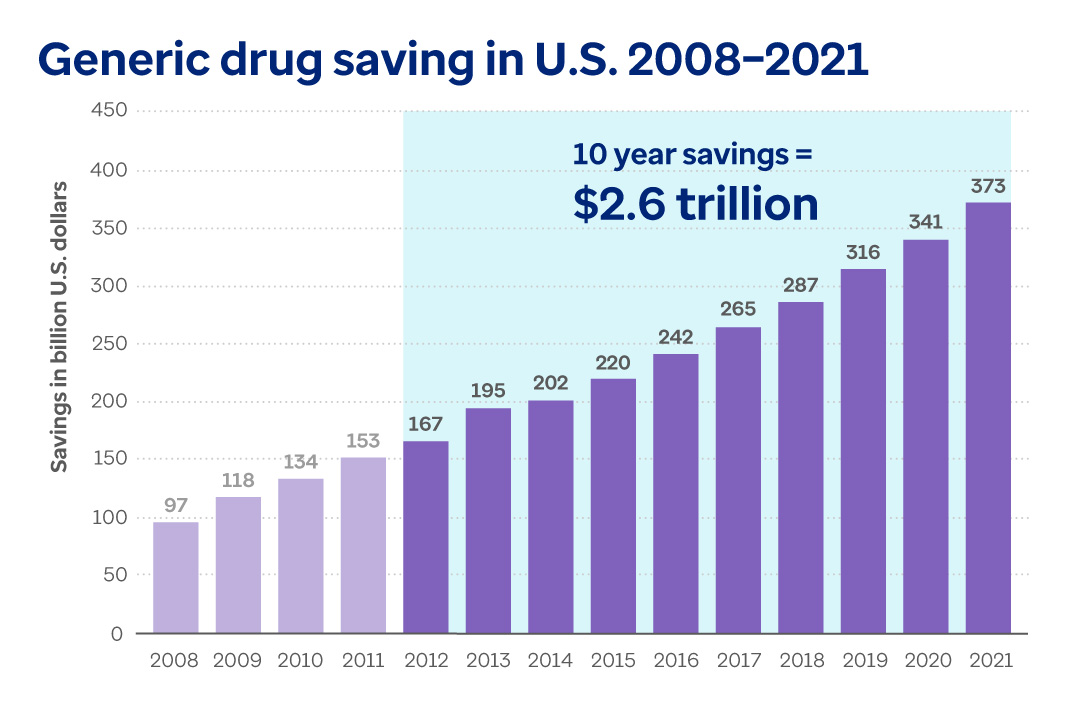
Since only drug manufacturers have the power to set drug prices, PBMs are the only counterweight to high drug costs in the healthcare system.
In order to bring some clarity to this discussion, let’s look at the facts.