Data that drives impact
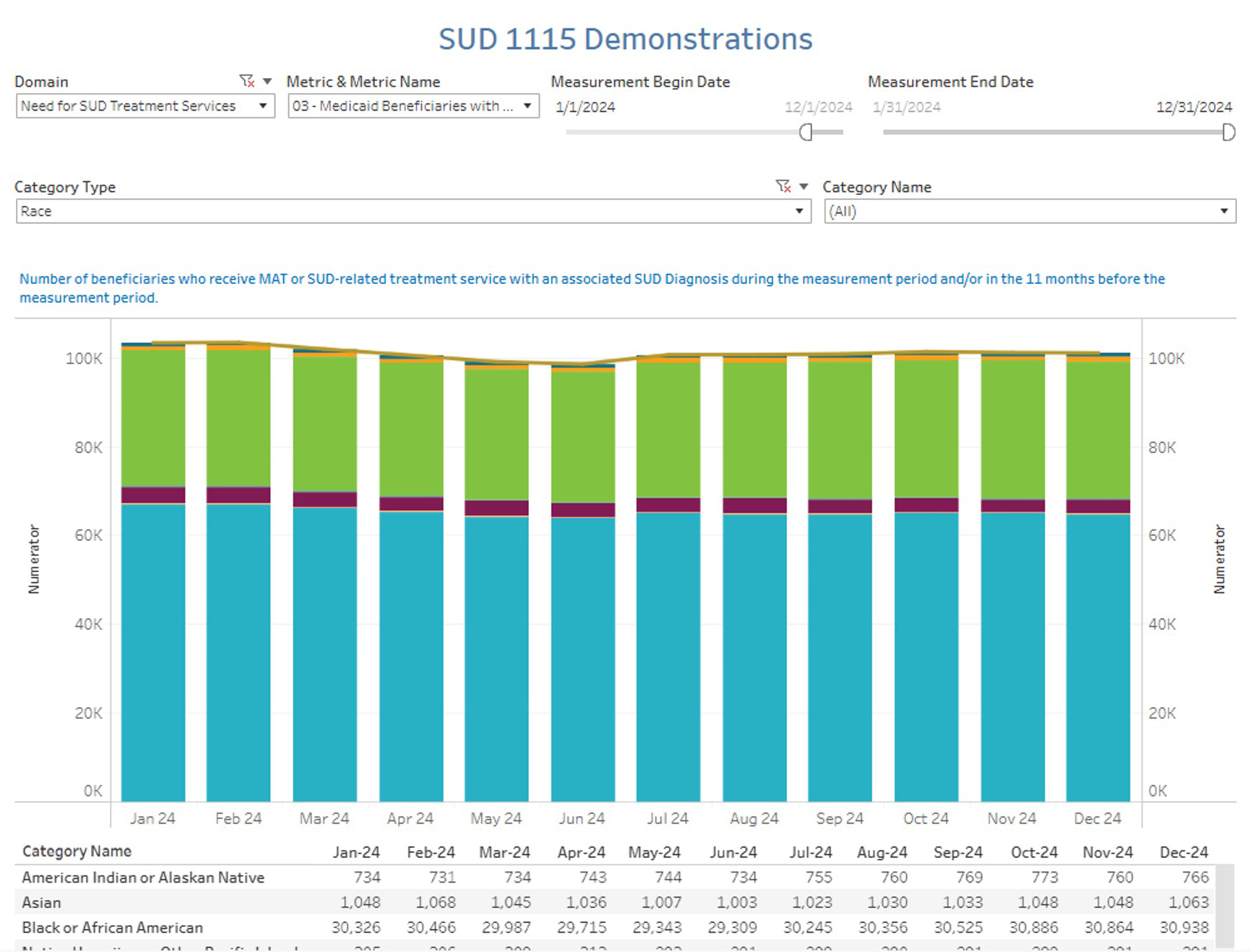
Substance use disorders (SUDs) affect millions of Americans, impacting individuals, families and communities. State and local investment in SUD treatment is essential, as it supports vital services like inpatient rehabilitation and outpatient counseling provided by specialized facilities and community programs.
By investing in treatment infrastructure and expanding access through Medicaid and other public programs, states can lower long-term healthcare costs, improve public safety and support recovery for individuals and families affected by substance use. Yet providing these resources is difficult.
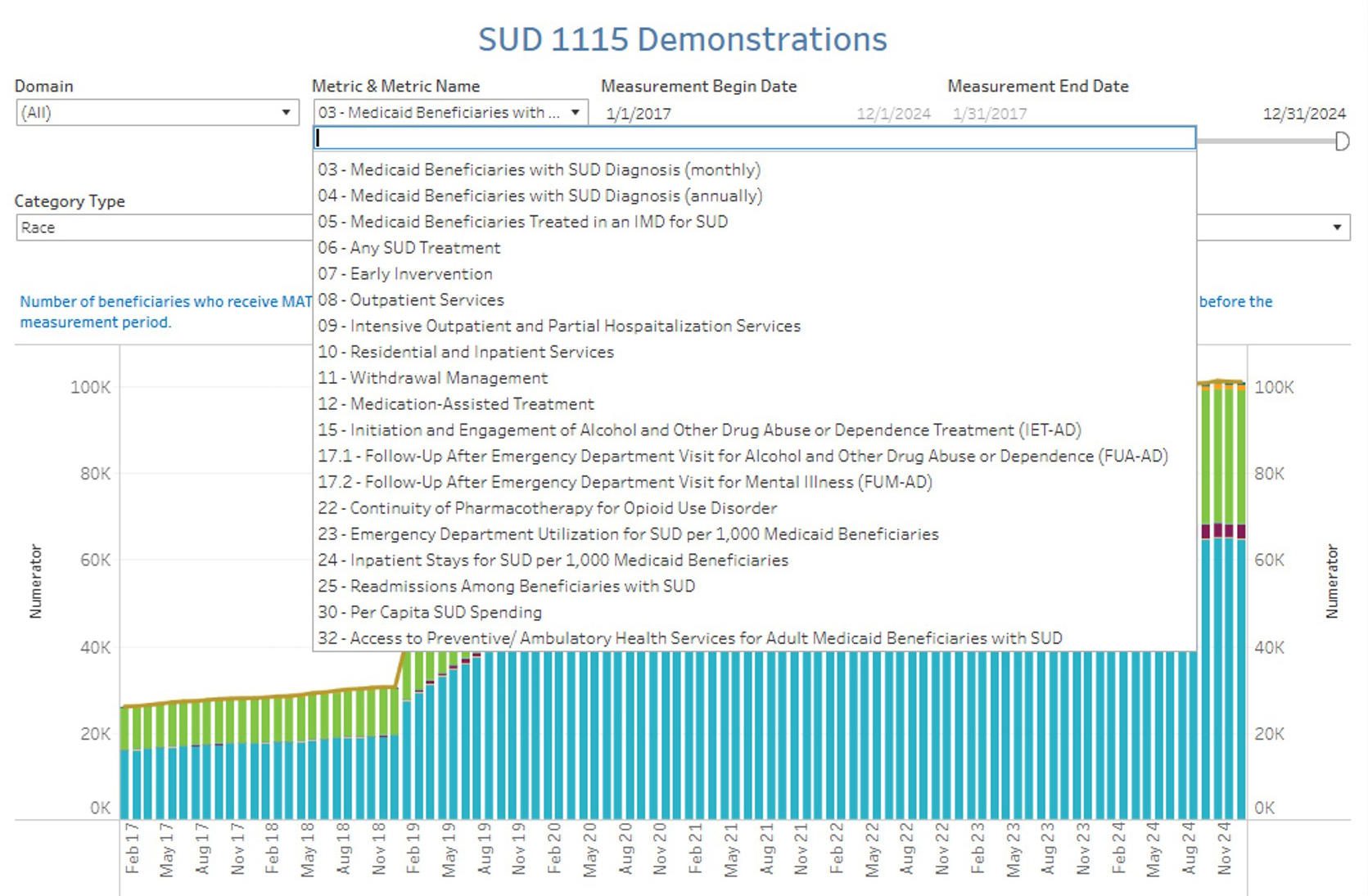
State policymakers must gather data from multiple often disconnected systems to understand the local impact of substance use disorders. With improved data coordination, states can strengthen community efforts to prevent substance misuse, expand treatment capacity and help vulnerable populations.