Get your patients the medication they need
Insurance denials are a common obstacle for many patients. Even patients who desperately need medication can be denied by their insurance company. That’s why our pharmacy appeals team is so critical.
With more than 100 years of combined experience, our clinicians, nurses and administrative experts work together on your patients’ behalf. Our team overturns greater than 8 out of 10 denials.

Key benefits
Our team helps you and your patients in several ways.
Customized appeal letters
Dedicated registered nursing staff reviews patient clinicals, investigates the insurance denial, and drafts a custom letter of medical necessity.
Second level assistance
We offer second level appeal assistance if needed.
Peer-to-peer review
We provide talking points to help you with peer-to-peer review.
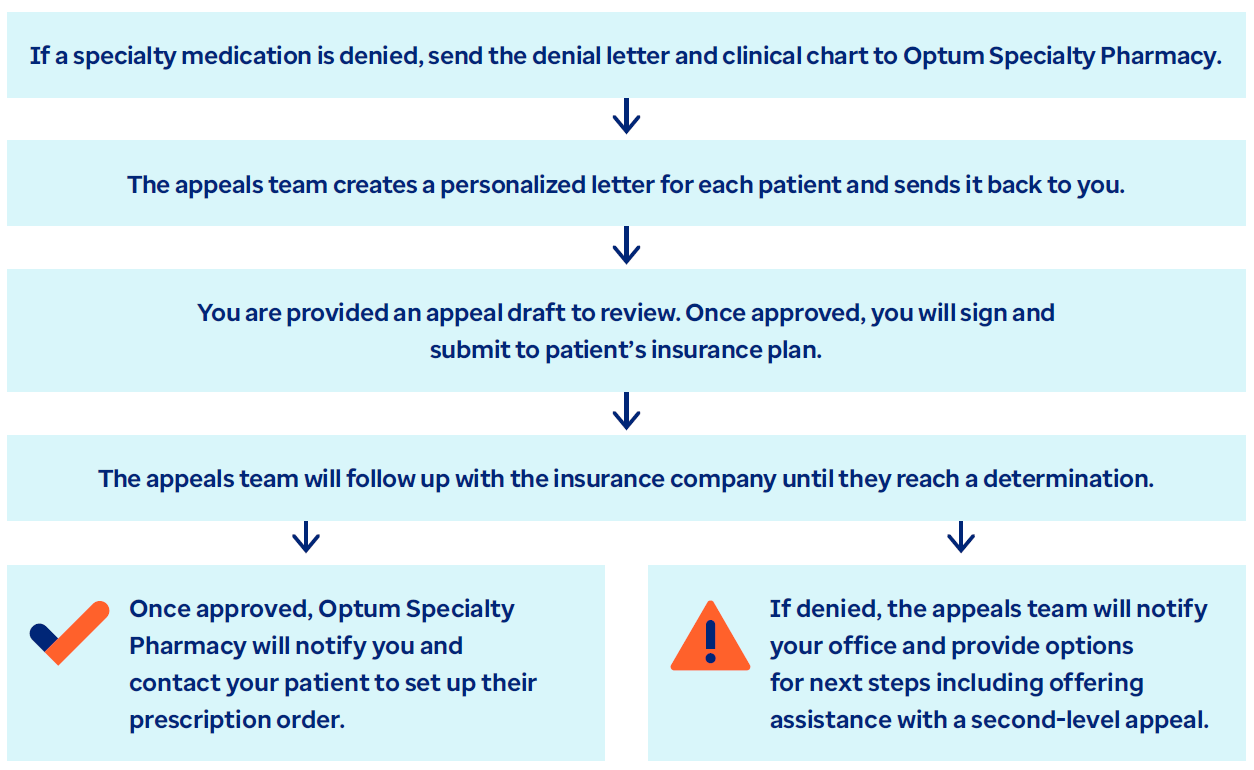
How our appeals drafting service works
Contact us
optumspecialtyappeals@optum.com
855-215-0235, Option 8
877-342-9352
Industry insights

Article
Learn about 5 strategies for consistent medication use and how Optum Specialty Pharmacy can help.
![Trusted Specialty Pharmacy Support [Video]](/content/dam/optum-dam/resources/videos/business/specialty-awareness-provider/specialty-awareness-provider.jpg)
Video
Optum Specialty Pharmacy simplifies prior authorizations, offers patient support and helps you save time with digital tools.

Article
In today’s healthcare landscape, the introduction and increasing use of biosimilars offers a promising solution to rising medication costs.

