Background: CMS Core Sets
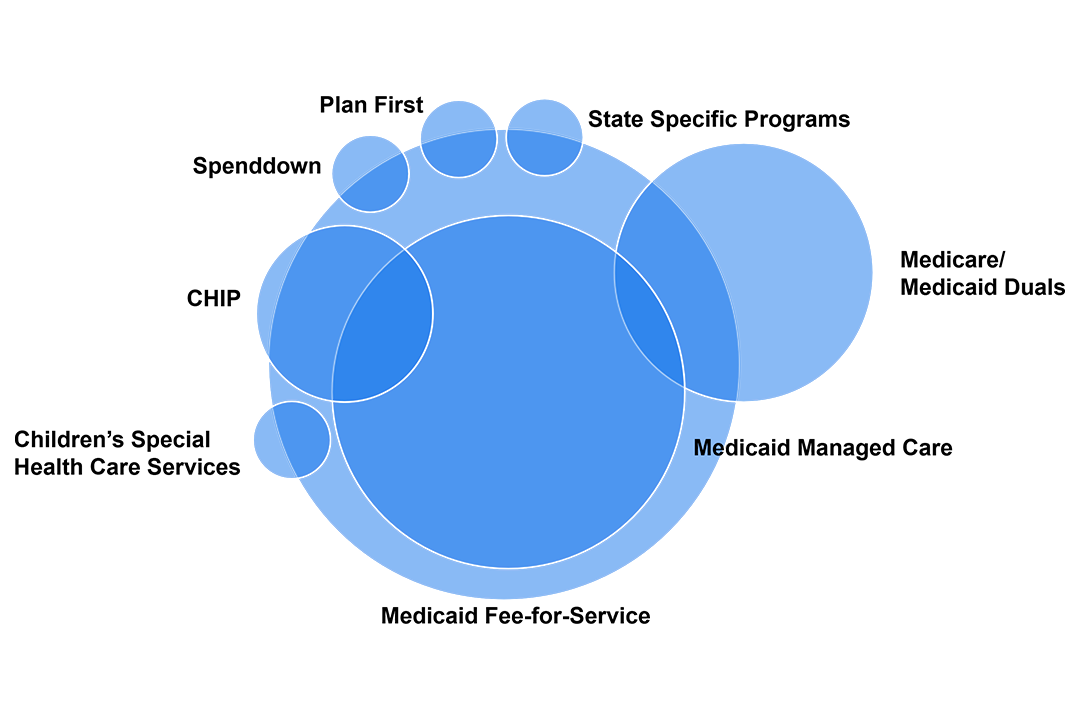
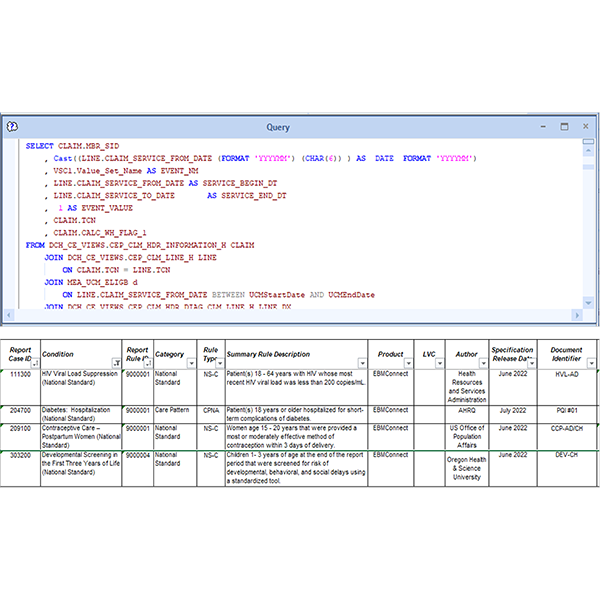
State Medicaid employees know CMS’s Child and Adult Core Sets — standardized measures tracking care quality for Medicaid and CHIP. Reporting, once voluntary, became mandatory for all states in 2024 to improve care and health outcomes.
At the 2025 State Healthcare IT Connect Summit, presenters from Optum and 2 partner states shared their experiences complying with the new CMS mandate. For each state, the different approach led to a shared outcome: enhanced cross-sector relationships that support quality improvement, care coordination and closing gaps in care.
Experts included:
- Yamini Raju, Data Analytics Manager, Virginia Department of Medical Assistance Services
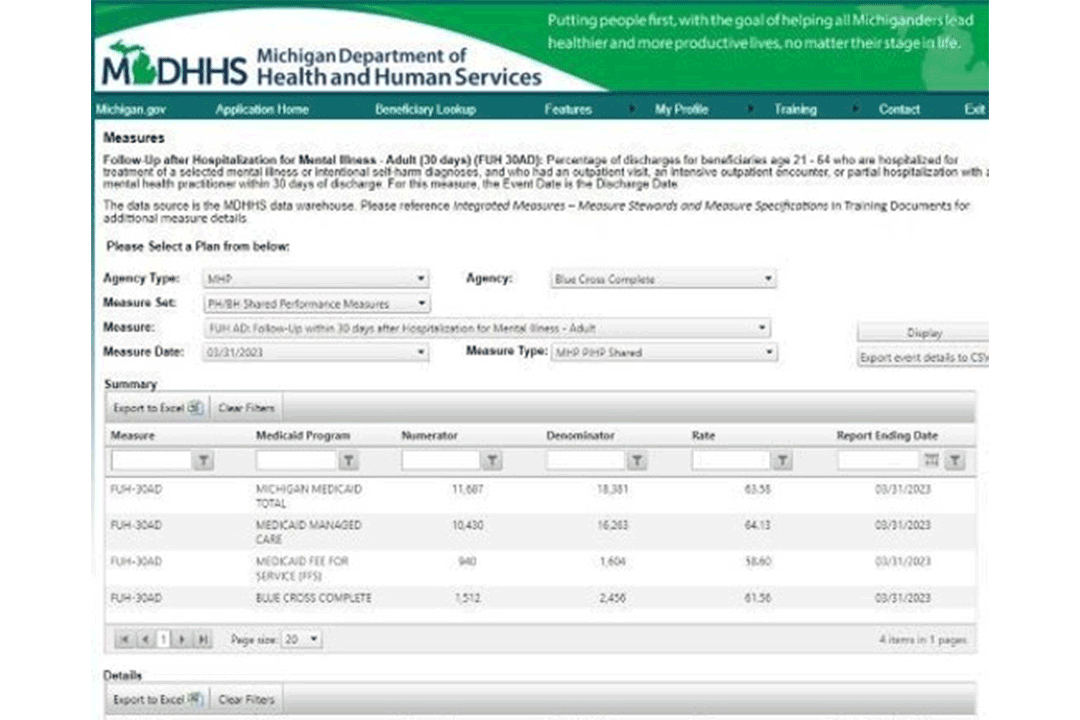
- Kasia Gruszka, Quality Improvement and Program Development Manager, Michigan Department of Health and Human Services
- Meta Kreiner, Population Health Specialist, Optum State Government Solutions
CMS Adult and Child Core Sets are federally mandated health care quality measures for Medicaid and CHIP. They were established under the Social Security Act to promote national standards for reporting and improvement.
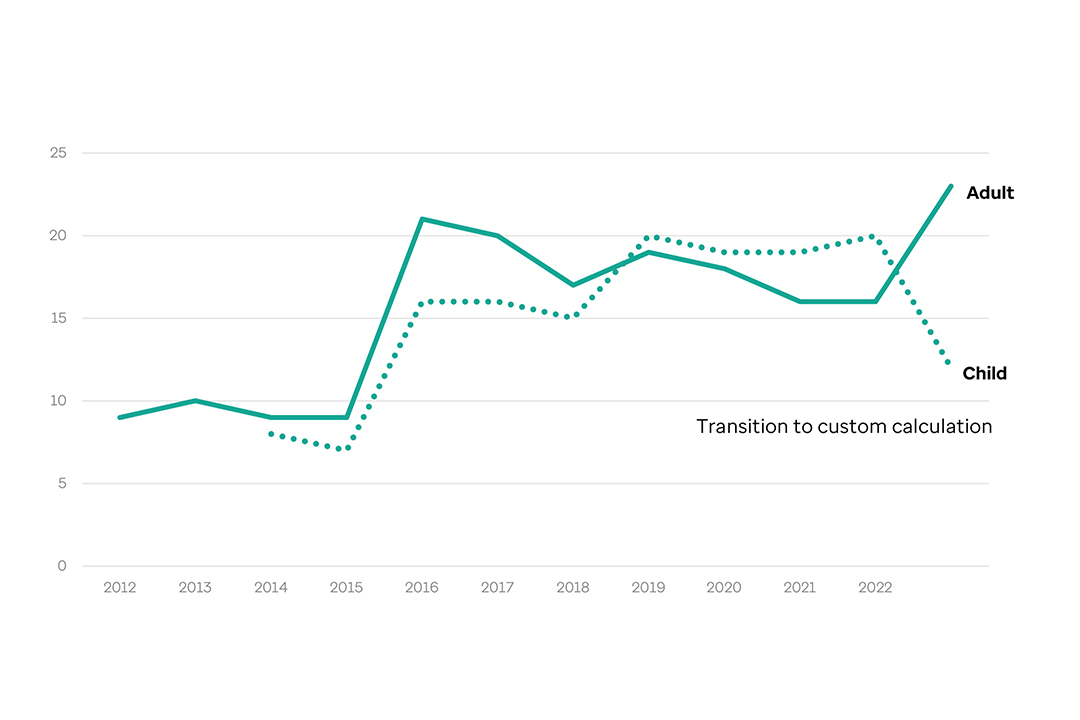
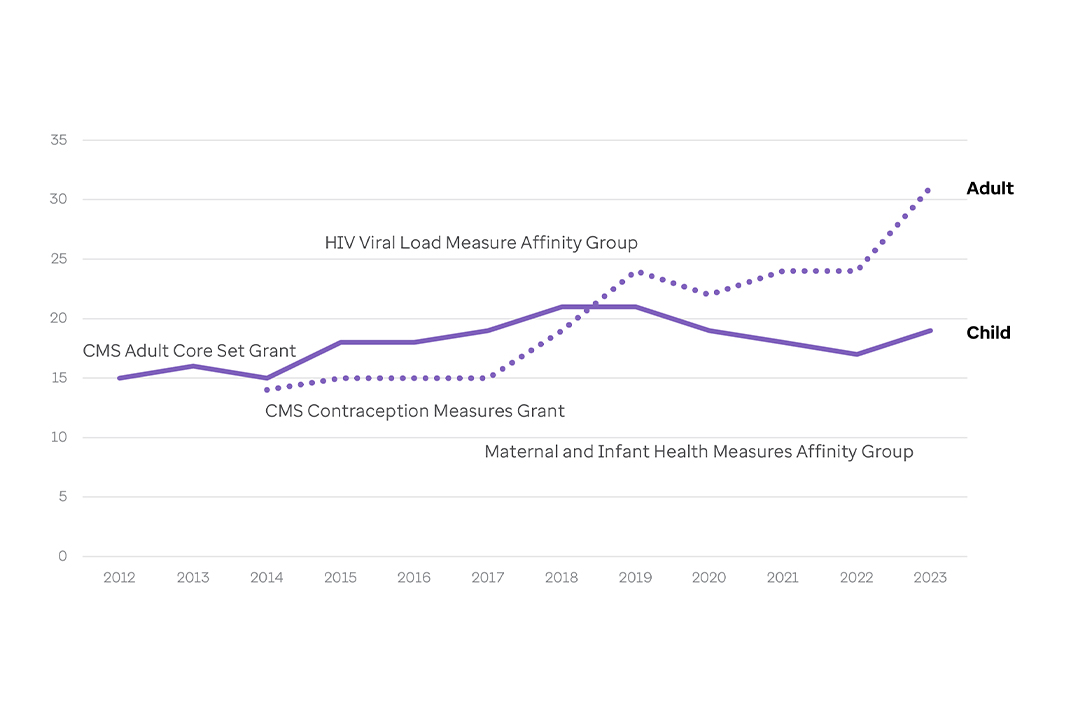
The Child Core Set launched in 2011 and was followed by the Adult Core Set in 2012. Reporting was voluntary until 2024, when it became mandatory for all Child Core Set measures and Behavioral Health measures in the Adult Core Set.
CMS updates the measures and specifications annually to reflect evolving priorities and evidence-based practices, for better relevance and impact across Medicaid and CHIP programs.
States must submit data annually. CMS publishes results for measures reported by at least 25 states that meet quality standards, helping benchmark performance and identify improvement areas.
In 2024, CMS launched a public dashboard featuring 2022 data from voluntarily reporting states. It shows national medians and state-specific metrics to guide health outcomes improvement.