Focused analytics help states discover wrongful activity
Home delivered meals offer a convenient, healthy way to support a patient’s recovery, provide proper nutrition and help manage chronic conditions. Several companies offer online ordering and delivery of fully prepared, refrigerated meals to Medicaid beneficiaries in their homes.
But what if the member is in the hospital or nursing home? How would the company know to stop delivery?
Would your state detect that meals are being delivered to a member’s home while they’re in a facility?
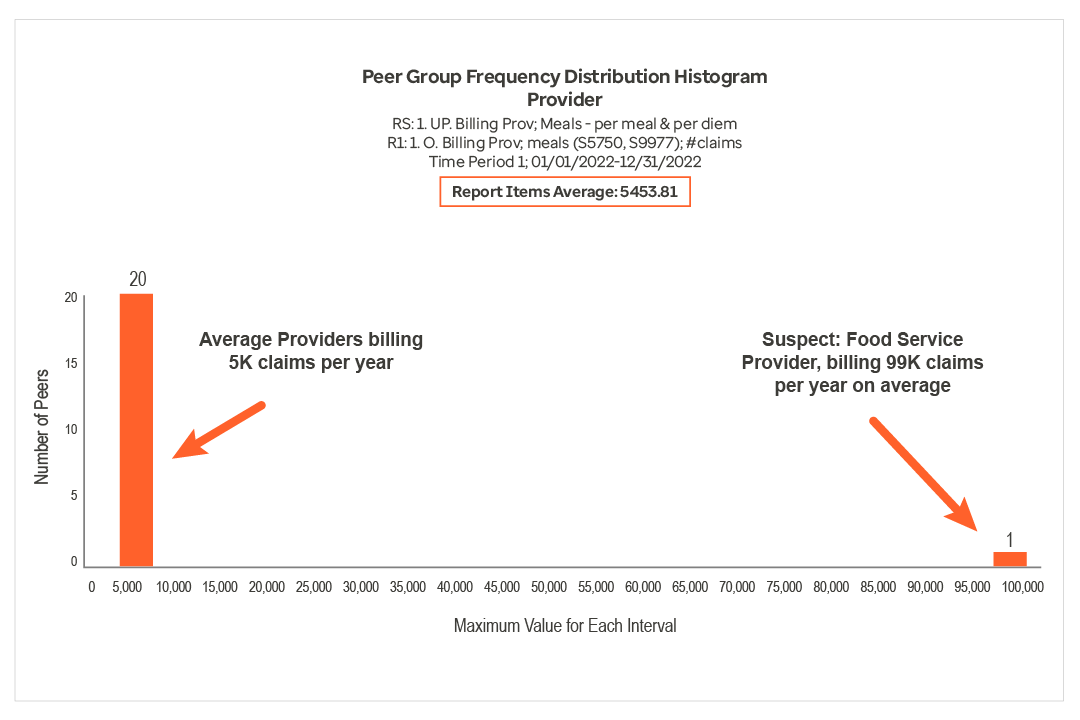
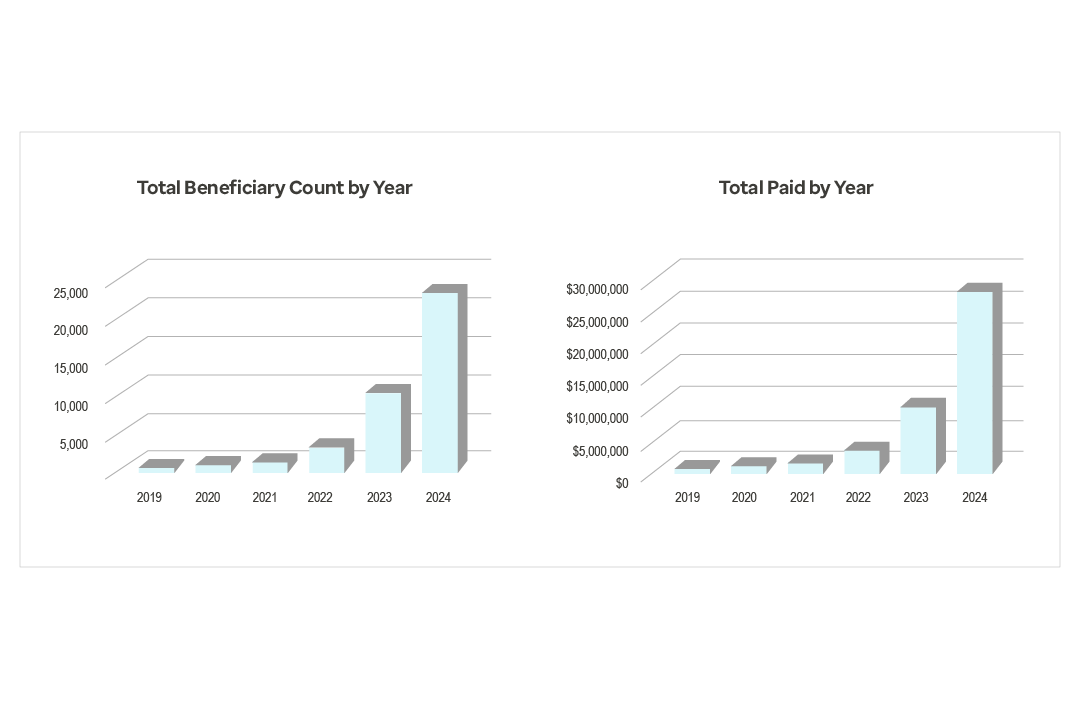
In 2024, customized analytics revealed fraudulent activity by a meal delivery service that led to significant savings for one state and identified mismanagement in other states.