What should you evaluate that you aren’t already looking at?
Getting a drug to market requires robust evidence and planning, no matter your company’s size. And many companies struggle with the same roadblocks, regardless of their market footprint or therapeutic area.
But small and emerging biopharma organizations have additional incentive to get ahead of things. Your organization has the same jobs to get done as larger companies throughout the product lifecycle. Still, there’s a different level of pressure to compete and differentiate your product, often with limited resources.
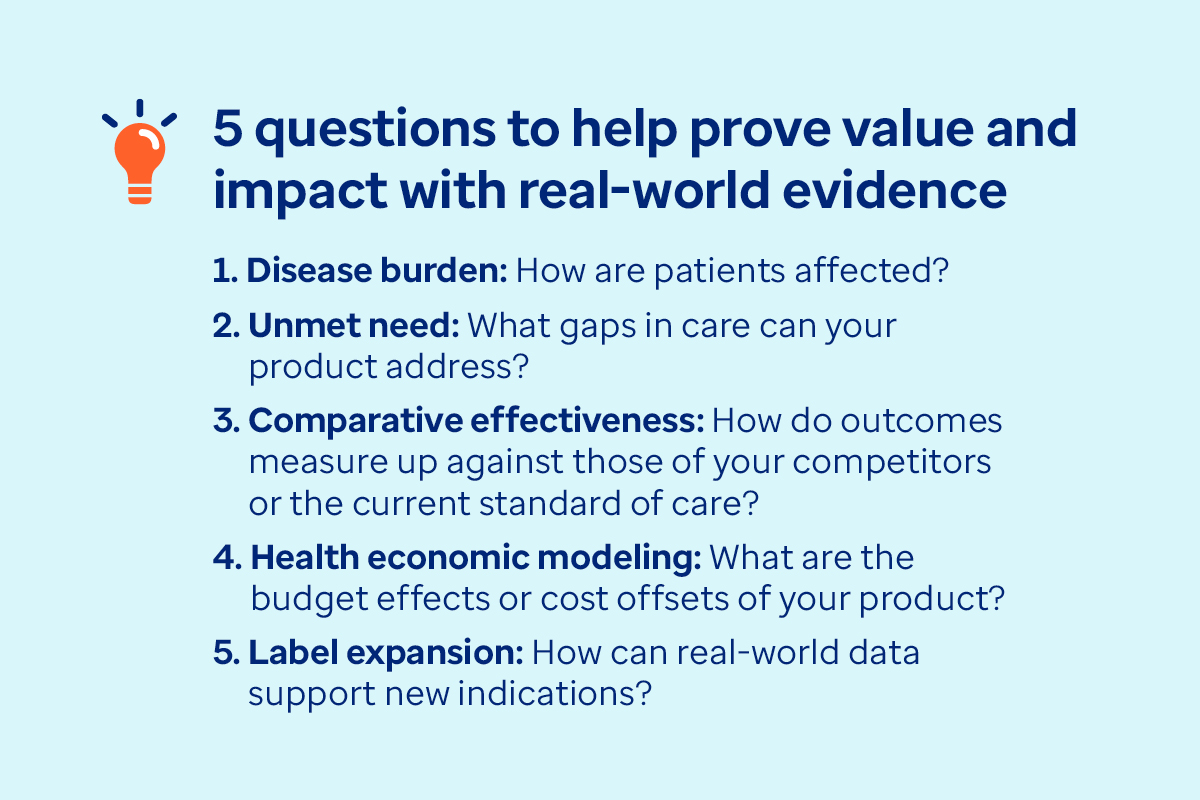
There are several steps you can take to generate evidence that your stakeholders — the U.S. Food and Drug Administration (FDA), payers, healthcare providers, consumers and policymakers — will need to support their decision making. To demonstrate the clinical, economic and societal value of your product, various health economics and outcomes research (HEOR) studies can help you address your toughest research questions.