Powered by Crimson AI
Assess care quality at a deeper level
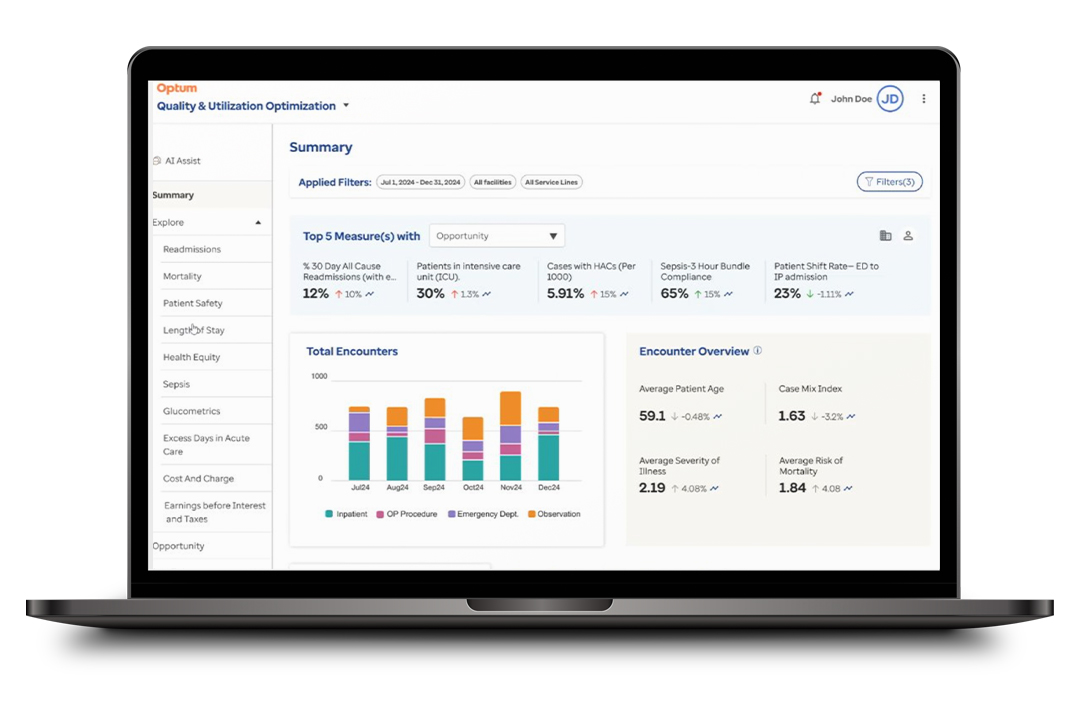
Powered by the Crimson AI platform, Quality and Utilization is a module that delivers outcomes-based analytics that help health systems better manage patient conditions, reduce readmissions and length of stay, and make the most of resources amid growing hospital utilization.
Improve quality and adherence to regulatory requirements through proactive outcome tracking and identify high-cost drivers or unwarranted resource utilization.
Key features
AI-enabled smart opportunities
Spend less time on mining data, and more time on generating insights. AI technology provides actionable feedback and suggested interventions that guide you to opportunity drivers. Proactively create custom EMR alerts based on these opportunities and quality initiatives.
Flexible reporting
Drill down, slice and pivot data with our advanced reporting capabilities built on PowerBI™. Our unified data mart integrates previously isolated data streams for scalability and customization. In addition, you can conduct analyses within your own data warehouse with our data portability functionality.
Regulatory tracking support
Gain access to our robust library of over 1,000 performance measures that leverage near real-time clinical and billing data. In addition, Quality and Utilization offers augmented national benchmarking capabilities and proprietary risk adjustment methodology.
Guided workflows
Our streamlined user interface makes it easy to identify opportunities and measure performance across key quality, safety and utilization metrics. You can drill down to view trends by facility, service line or physician and even dive into encounter-level details.
Active data management
Perform a deeper analysis of care quality with our solution. Quality and Utilization processes clinical data daily and unifies data previously isolated in different workstreams. It even delivers responsive, interactive reports based on this live data.
Key benefits
Discover how the Quality and Utilization module can improve patient outcomes for your healthcare organization.
Improve quality outcomes
Enhance patient safety and quality outcomes across your health system.
Optimize resource utilization
Optimize utilization of resources by identifying high-cost services that may be unwarranted.
Pinpoint documentation opportunities
Equip your team with robust quality indicators, social determinants of health (SDOH) data and our risk-adjusted benchmarks to help your physicians and CDI teams improve documentation.
Our impact
Optum has helped its clients achieve impressive outcomes and major cost savings.
26% reduction in sepsis mortality rate
Quality and Utilization has helped CommonSpirit Health reduce its sepsis mortality rate by 26%.1
6.3% reduction in sepsis length of stay
This solution has reduced length of stay by 6.3% for CommonSpirit Health.1
5% reduction in readmission rates in one year
Optum helped one of its clients reduce readmission rates by 5% in just one year.1
$99 million in cost savings
We've helped clients achieve close to $100 million in cost savings associated with hospital quality and resource utilization initiatives.2
Industry insights
![Improving Hospital Quality & Utilization [Case Study]](/content/dam/o4-dam/images/professionals/health-workers-discussing-results-1080x720.jpg)
Case study
Learn how data insights helped 4 organizations transform their operations.

White paper
Learn more about how Crimson AI enables best practices for achieving operational excellence.

E-book
Optimize your provider review process to help save time, reduce costs and improve care quality.
Product information and resources
-
Download now
PDF
Fact sheet
Quality and Utilization fact sheet
Learn more about this product’s key features, its modules and client impact to date.
Complementary solutions
Crimson AI Provider Review
Streamline physician review management and improve provider engagement with a unified AI-enabled workflow tool.
Crimson AI Surgical Cost Module
Enhance surgical service line profitability by utilizing data-driven insights to streamline costs and improve efficiency.
Crimson AI Surgical Capacity
Optimize surgical scheduling and operating room utilization with data-driven analysis and insights.
Crimson AI
Unlock healthcare data and transform it into robust business intelligence using AI-enabled feedback and suggested interventions.
Sources
1. Based on mutually agreed on ROI between the client and Optum.
2. Based on mutually agreed on ROI from all clients across 2019–2023
